Category: Uncategorized
More Bruckner
Bruckner Symphony No. 3 in D minor and Symphony No. 4 in E-flat major
Bruckner, Mahler, Sculthorpe in transit
A few bits and pieces I’ve been listening to:
Mahler 1
Bruckner 1 & 2 in C Minor
Peter Sculthorpe – Sun Music
Things they didn’t teach in medical school: Part 24 Innovation
This is a brief post that needs some more thought and input. This week I’ve been attending @TEDMED at the Kennedy Centre in Washington. Naturally a major theme is innovation. Start-ups, entrepreneurship, thinking out of the box and radical re-thinking is being showcased. Successful entrepreneurs were asked to speak about innovation: interestingly it is common that they can’t explain how it is done (or they are modestly protecting the secret). So if innovation can’t be taught then why include it in the ‘Things they didn’t teach in medical school’ series?
Innovation is a fancy name for making things better. This is perhaps beyond quality improvement and extends to recognising there is problem that requires fixing and then identifying a solution. There is no shortage of problems that innovative ideas could fix in hospitals.
When I attend medical conferences one thing I frequently observe is that people (doctors, nurses and other members of the healthcare team) often have great ideas for solving problems. What the real problem for innovation in healthcare seems to be is a large number of artificial barriers, sustainability, reduction of duplication and dissemination of the big ideas.
An example of the barriers is the IT department. When my colleagues first suggest using Moodle (a learning management system) for the purposes of orienting and training our registrars they were blocked. IT wouldn’t let the external site be accessed through the firewall. Later on the hospital actually adopted Moodle for its’ organisational learning program. Another example is new forms required for safety projects might take months to approve though the ‘forms’ committee.
Ofter innovations are led by a champion who has a short term grant to undertake an improvement project. There is short term success and then when funding runs out the champion, by necessity moves on. In the same way you might find exactly the same project undertaken at another hospital.
The other important barrier is a lack of parties willing to provide opportunity. Start-up companies go and look for venture capital. In hospitals, especially in the public sector, there is no equivalent of venture capital. Convincing administrators to invest in your idea is not easy.
Dissemination of innovations has all sorts of barriers put up by organisations – more often than not these objections are based on money, however, one of the problems is doctors and other healthcare professionals have never been trained how to best undertake organisation and behavioural change: perhaps this is the real skill that hasn’t been taught in medical school – and this will be discussed in the next post.
Tippett Suite for the Birthday of Prince Charles
Michael Tippett Suite for the Birthday of Prince Charles played by the Chicago Symphony and Sir George Solti
Things they didn’t teach in medical school: Part 9B Self-management – or perhaps self-assessment
So perhaps this should have been part 20.
Assessing one’s own performance as a doctor is not taught at medical school.
The problem is of course that as a doctor there is a touch of the ‘God’-complex, not to mention a historical lack of scrutiny.
But on a more personal note it is actually very difficult to step-aside and assess your own performance objectively.
One way to do this is to focus on how you handled the difficult case. But in reality the difficult case was probably going to be difficult regardless of how brilliant a clinician you are and in many circumstances the reasons why the case is difficult is out of your control.
I think the real challenge is assessing overall performance. A little like assessing organisations you can assess processes and outcomes. Outcomes are the difficult measure because you don’t necessarily know how your peers perform and different doctors treat patients with different ‘degrees of difficulty’.
For both process and outcomes you can assess against benchmarks and guidelines but there will always be uncertainty about how these are set.
Finally one needs to have a personal reference point: do you aim for a consistent standard within a specific set of skills or do you have a reference of achieving both this, combined with progressive improvement & expansion of your skill-set.
I think the latter is the most important issue that needs to be addressed before the profession can embrace personal self-assessment. Do the practitioners know what their goals are? Do you graduate and coast or graduate and grow? Self-assessment needs concrete actions otherwise others will do it for us and no doubt in a way that won’t be helpful.
Mahler Symphony No.4
Lorin Maazel conducts the New York Philharmonic in Mahler Symphony No.4
Hindemith Symphonic Metamorphoses on Themes by Carl Maria von Weber
Paul Hindemith Symphonic Metamorphoses on Themes by Carl Maria von Weber played by the Philadelphia Orchestra conducted by Wolfgang Sawallisch
Things they didn’t teach in medical school: Part 17 Stuff nobody taught the patients
So this is a bit of a spin on the health literacy and communication problems I’ve previously commented on. One of the things that wasn’t taught in medical school is what the patients don’t know. Now at one level this seems obvious – I went to medical school to learn the stuff that you need to know to be a doctor and that separates the doctors (& nurses) from the patients. In fact we get taught all of the medical stuff but we aren’t taught what the patient’s understand.
Here are some comparisons:
Patient: A no sugar diet will starve the cancer
Doctor: Your body will put whatever you put into your mouth into sugar
Patient: Does freezing or drying deplete the anti-oxidant powers of blueberries?
Doctor: There is no evidence that anti-oxidants are beneficial – and they might be harmful
Patient: The cancer still might be curable (even though the patient is bed bounds and is on 3rd line therapy and has widely metastatic disease)
Doctor: The cancer isn’t curable and we can hope to provide good palliation
Health literacy is a big problem and it goes beyond reading the label on a prescription. Understanding illnesses, understanding the information on the internet, navigating the health system (making appointments & paying the bills) are all part of health literacy. Doctors need to know what their patients (& carers) don’t and help teach them.
Things They Didn’t Teach in Medical School: Part 16 Discussing Death
One of the things that wasn’t taught very well in medical school was talking about death. Once you start being a doctor you get confronted by this conversation pretty quickly and very frequently. Some get the hang of it and others don’t. Some avoid it.
But let’s deal with reality. Most doctoring is about prolonging rather than saving lives and everybody is one day going to die (something that doesn’t seem to be taught anywhere). So talking about death is a conversation that has to be had.
Unfortunately there is a common belief that talking about death is talking about stopping or not having treatment. This is certainly not the case. This discussion is about how and where a person wants to die. More often than not the ‘when’ is not controllable.
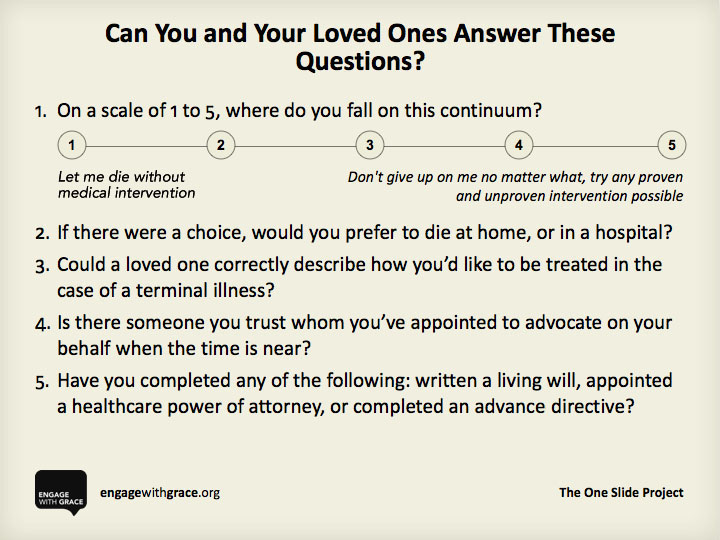
Right now there is a great deal of formal work being done around Advanced Care Directives. But there is a also a broader community movement starting to have the conversation. Examples in the online community include http://www.deathoverdinner.org and http://engagewithgrace.com
Engage with Grace is promoting The One Slide Project – an idea to get people thinking about 5 simple questions. Here is the slide – start having the conversation.
Glass Symphony No.8
Philip Glass Symphony No.8, Bruckner Orchester Linz, Dennis Russell Davies
